One in a Million
Written by Sam's mummy, Rachel.
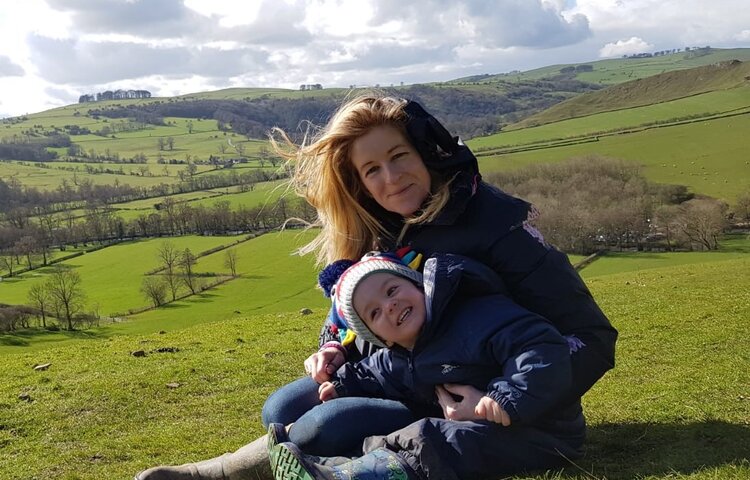
Sam, my darling son, was a precious and much loved little five-year old superhero. He was a very healthy little boy, had little in the way of illnesses and was very fit. Sam loved the great outdoors, from cycling for miles on his bike with his daddy, going on long walks with Daisy his beloved dog, playing in mud and streams, finding sticks so he could turn them into anything that happened to capture his imagination, collecting stones to fill our pockets with, to finding the best puddles to jump in. Sam loved Lego, superhero toys, his wooden train set (he set up train tracks all over the house), monster trucks, and dressing up in one of his many costumes.
He was kind, gentle and loving, and was shy until you got to know him. Sam loved to please people, make people laugh, use his imagination, and had a real thirst for learning; he was so articulate even from an early age. Talking to Sam was like talking to someone five years older; he was so wise for his years. In case you haven't quite yet grasped it, Sam was an utterly dream little boy. I was incredibly blessed to have been chosen as his mummy.
The Day Our Lives Changed Forever
On Monday evening 22 March 2021 at 8pm, every parent's worst nightmare came true and our lives irreversibly changed forever when Sam had his first ever seizure. In fact, this nightmare was far worse than anyone could ever imagine, it was certainly not one that had even entered my conscious thought process.
Over the weekend of the 20 March Sam had a very high temperature, slight sickness and lethargy. We sought advice from the different out of hours services over the weekend, and it was put down to Sam having some sort of virus. On Monday morning I contacted our GP, who again felt that Sam had a virus and to continue giving him Calpol and Ibuprofen. Late Monday afternoon as Sam's temperature was still high (though he had been relatively fine in himself on Monday afternoon and had been playing at his grandmas) I started to panic and so I took Sam to Derby Walk in Centre. Sam had an examination and nothing of any significance was identified, they felt Sam had a virus. However, they prescribed penicillin as a precaution, as his throat was red and he had a history of tonsillitis.
After a quick diversion to the late night chemist for penicillin we got home around 7.45pm. I gave Sam his first dose of penicillin as soon as we got home and I then asked him if he would like a drink of water. He said "no mummy", which I did think odd after having medicine. These were the very last words I would ever hear my son speak. As Sam sat on our kitchen table I noticed he was drooling and blowing bubbles and didn't respond to me when I asked him what was wrong. I immediately phoned his Dad who had only just left us, and asked him to take us to A&E, I cannot begin to say how panicked I was. After I put the phone down, Sam collapsed unconscious into my arms.
I immediately phoned 999 whilst scooping Sam up into my arms and running to my neighbours house. All the way I was screaming for help. To say I was utterly panic stricken would be an understatement. At my neighbours we lay Sam on their sofa, and he remained fully unconscious having seizures for over 30 mins.
East Midlands Ambulance (EMA) arrived within around 10 mins. Sam finally stopped seizing around 8.35pm and was transferred to the ambulance. We were blue lighted to hospital and the paramedics gave a pre-alert to expect our arrival. In the ambulance I knew that something was dreadfully wrong with Sam, call it mother's intuition. Whilst he was sat up in the ambulance with his eyes open, he was not talking, he was not distraught, he was not crying, he was not reaching out for me. He should have been petrified, but he was not making a sound. I now believe that he was unable to talk, it was clear something was catastrophically wrong.
Derby Royal A&E
We got rushed to Derby children’s A&E where I was obsessed about Sam having antibiotics as I was thinking he had an infection. In A&E Sam preceded to have further two seizures (which were excruciatingly painful to watch). His airway became severely compromised during the seizures, and his oxygen levels plummeted. After his first seizure in A&E he came round i.e. his eyes were open, but he was still not talking and not reacting to anything around him. After his second seizure, he didn’t wake up but seemed to be in a very strange deep sleep. I was told that this was commonplace after having a seizure. Sam had a head scan whilst we were there, which showed nothing significant. To say I was panic stricken and beside myself with fear and worry about my little boy would be an understatement. It was fear like I had never ever experienced before.
Derby HDU
Sam got admitted to HDU in the early hours of the morning, and I stayed with him. During the night, Sam started having further seizures, and he began having trouble maintaining his airway and was becoming hypoxic (lack of oxygen). I could see the medical team were panicking, and that is not in any way disparaging to them. The nurses were doing their best in a terrifying situation, and I was utterly beside myself. It was clear something was catastrophically wrong with Sam. I wasn't made aware at the time, but have since learnt that Sam went into respiratory arrest at around 2.45am in the morning, they believe it was a side effect from the medication they had given him. As a result more and more medical people were coming to help Sam, and he ended up with a huge team around him. I was simply terrified I didn’t have a clue what was happening. I now know that they were arranging for him to be placed into an induced coma and intubated to help him maintain his airway.
Once Sam was placed into an induced coma the Derby team sought advice from the CoMET (Children's Medical Emergency Transport Team) so he could be transferred to the PCCU (Paediatric Critical Care Unit) at Queens Medical Centre Nottingham, which is a specialist neurology centre, around 20 miles away. Once a child needs intubating they need to be transferred to a more specialist hospital. We didn't know it at the time, but the team at QMC are people we would grow to enormously respect and trust and would prove instrumental in Sam’s care over the coming seven weeks. We are forever indebted to them.
Meeting the Super-Hero CoMET Team
The CoMET Team arrived around 5am that morning. When they walked in to HDU, they had this calmness and utter professionalism that I was blown away by. Straight away I knew that Sam would be in safe hands, they were like a team of real-life superheroes. It took them around five hours to stabilise Sam and prepare him for transfer.
When Sam was ready for transfer, it was like an out of body experience to see my precious boy surrounded with drips and electronic equipment to keep him alive. His transport trolley was essentially a mobile intensive care unit. Myself and Sam's dad walked with him and his transport team to the waiting ambulance. We weren't allowed to travel with him; there was not enough room for everyone in the ambulance, and we were given strict instructions that we must not try and follow the ambulance. Can you imagine the thought of your child being blue lighted to another hospital without you being there next to them? So in utter shock at how life had come crashing down on us we rushed home to pack overnight bags and make our way to Nottingham’s Queens Medical Centre. Little did we know just what truly heart-breaking and devastating times lay ahead for Sam.
Entering the New World of PCCU
We entered the alien world of PCCU around midday, and it was terrifying, we were distraught, we were in shock, we had no idea what to expect and what lay before us. Sam was placed into isolation, as it was still uncertain whether COVID-19 had a part to play in this, or indeed if he was still testing positive for COVID from myself and Sam caught it just before Christmas 2020. We were extremely fortunate that we were given a parent's room to stay in, which was just 30 seconds away from Sam’s ward, and we feel forever grateful for this.
What was Wrong with Sam?
From our initial chat with the PCCU consultant team, we felt positive that these seizures could be treated and stopped. It was thought that they were being caused by a virus, or infection. Apparently, there was a huge protocol of anti-seizure medication that could be given to Sam, and we felt optimistic. He was in the best possible place; he was on antibiotics and anti-viral meds to treat underlying causes.
Whirl Wind of Activity
For the first couple of days there was a whirl wind of activity around Sam. There was a constant team of people making up new IV bolus medications. Medications would initially work, but then his brain would find a way round them and he would start to seize again. It was utterly devastating and heart breaking. I was terrified, an emotional wreck and in pieces. Alarms were repeatedly going off, either from early warnings on his vital signs such as BP, heart rate, or breathing, or from alerts that medications required changing. He had a huge number of medications going into his tiny body. I felt permanently petrified that I was going to lose my son, and have never felt fear like it in my life.
A CFAM (Cerebral Function Analysis Monitor) device was attached to his head, to monitor his brain activity, alongside continuous visual recording of his body to help identify clinical seizure activity.
The medical teams were making their way down the anti-seizure medication protocol, the further they got down it, the more toxic the medication was. Sam was now in Super-Refractory Status Epilepticus territory. Refractory status epilepticus is seizures that persist despite administering two anti-seizure medications. Super-Refractory Status epilepticus is seizures that persist for greater than 24 hours, despite anaesthetic treatment, or it recurs on an attempted wean of the anaesthetic regimen. It is a life-threatening condition, as seizures longer than 30 minutes can kill brain neurons, or in plain English they can cause brain damage. Sam's seizures HAD to be stopped.
Stopping the Seizures........ the Impossible Task
It soon became clear that stopping the seizures was not going to be straightforward. The first few days of Sam being admitted to PCCU are a blur. I was too panic stricken, anxious and emotional to even think straight, let alone remember anything. I was relying on his dad listening and communicating with the medical teams. I just kept thinking he is in the best place possible, you need to leave it to them Rachel, don’t start googling, trying to input into his treatment, trying to second guess, trying to micro-manage a subject that you know nothing about. You will send yourself crazy, it won’t be helpful and may even impact on Sam’s care.
No Room for Bystanders
As the realisation became apparent that stopping the seizures was proving not to be straight forward, I knew that Sam needed his mummy to fight alongside him. There was no room for bystanders. He needed a mummy who would work alongside the medical team, be his voice, who would fight with every breath and bone in her body to help find a cure for this catastrophic condition. And alongside my son, and the medical team that is what we did, we FOUGHT, FOUGHT, FOUGHT, FOUGHT FOUGHT. We were not giving up, indeed I would NOT allow anyone give up. I was like a lioness fighting to the death for her cub. I have never felt more protective of Sam in my life. Anyone who dared utter any negativity I was all over it. I needed to know and feel that everyone was 100% committed to Team Sam; to finding a cure, we would BEAT this.
One in Million Chance
We were soon informed by Sam’s Neurology team that what he was presenting with was an exceptionally rare condition called N.O.R.S.E. (New Onset Refractory Status Epilepticus) and F.I.R.E.S. (Febrile Infection Related Epilepsy Syndrome). We were given a printout from NORD (National Organisation for Rare Disorders). A rare disorder is something that no parent wants to hear their child has got. F.I.R.E.S. is a subcategory of N.O.R.E.S., and it is not a diagnosis but describes the symptoms that are being presented by the patient; it is a condition.
This syndrome is exceptionally rare, and heart-breakingly Sam had a one in a million chance of developing it. It is also extremely challenging to treat, there are no standard treatment protocols as it is so rare. We were therefore relying on the experience and knowledge of Sam's amazing neurology and critical care consultants. The underlying cause of these seizures was also yet to be identified, as it didn’t appear to be an infection such as meningitis, thus making it even more challenging to treat. It wasn't genetic as the tests we had done were all negative. It was basically like fighting someone blindfold.
Sam a Real-Life Super-Hero
Sam was placed on a huge mix of medications including a number of anaesthetic drugs. Some of these drugs are only for use in a critical care setting, are exceptionally toxic, and therefore should only be used for a short period of time. Sam was so amazingly strong, he ended up being on some of these medications for weeks, which would have proved deadly for an adult. He was surviving as he was young, so fit, healthy and his heart was so strong. Sam is truly a real-life superhero, to say I am proud of him, would be an understatement.
The anaesthetic drugs were aimed at suppressing his brain activity, so we could achieve what is called "burst suppression" for a period of 48 hours, i.e., stop all brain activity apart from an occasional burst approx. every 4 seconds. It was hoped that this would be sufficient to rest his brain, and allow it to reset, so we could then slowly restart it. Similar to a reset on a computer when it goes haywire.
Other innovative therapeutic treatments were given which were generally aimed at suppressing Sam’s immune system as it was felt this was a probable cause of his seizures i.e., his immune system was attacking itself. Some of these treatments had not been used in Nottingham PCCU before to treat these type of clinical symptoms.
Other Complications
During the seven weeks Sam was in hospital, he encountered many other complications and challenges, far too numerous to mention here. But included brain swelling, cerebral salt wasting with elevated urine sodium, severe constipation resulting in significant stomach aspirates and non-absorption of food through his enteral tub feeding, significantly high triglyceride levels (fat in the blood), unstable body temperature, infection, pneumonia, low blood pressure (which went too high towards the end), low heart rate (which went too high towards the end) etc.
He had an amazing medical team, and I felt he really was receiving world leading care. The teams were very engaging and open to input from us as parents, and they reached out to other medical centres and colleagues from not just within the UK but around the globe. There was no room for egos and the teamwork was first class. We were very much viewed as a very active part of the team caring for Sam. My fantastic sister-in-law, Amy, who lives in Denver was also frantically researching possible treatments, and she found articles on the use of Anakinra as a possible cure, which we ended up trying.
Stressful MRI Scan Days
Sam had four MRI scans throughout his stay, I hated these days, they were so stressful. From seeing him being transported with all his equipment keeping him alive, to receiving the results. The brain is the most complex organ of the body, and the least understood even in 2021. The one certain outlook, outcome or prognosis in all of this, was uncertainty.
A bad MRI scan did not necessarily correlate into a poor outcome. There were patients who had poor MRI scans which had minimal impact on them. Then there MRI scans which outwardly did not appear to bad, but where patients had poor outcomes.
Best Care Scenario - Significant Disabilities
Sam was initially booked for an MRI scan on the Wednesday, within 48 hours after his first seizure, but he was too unstable to go. Consequently, Sam had his first MRI scan seven days later. We received the results literally instantly, within minutes of him returning the ward. It was devastating. The best-case scenario for Sam was that he was going to have significant disabilities. He had a number of legions (damage) on his brain caused from the seizures. The second MRI scan showed brain swelling, from the seizures, which aligned with his pupils that had stopped reacting. We determinedly but tearfully told the team, we didn’t care what disabilities our boy had, we would give him the best life we possibly could. He would have a full-time mummy caring for him, who would make sure he had the best quality of life regardless of disability. They just needed to focus on keeping him alive.
As the weeks passed, at each MRI scan we would see the progression of these legions, which is where the brain tissue had died. It would eventually evolve and leave catastrophic 'holes' in his brain which would fill with pockets of fluid.
Daisy
We were exceptionally blessed to have an amazing team of consultants looking after Sam. They were everything that you needed them to be professional, calm, caring, open, engaging, innovative, compassionate, dedicated, committed the list is endless of the adjectives I would used to describe them. Around four weeks in, Sam's awesome consultant made arrangements for Daisy, Sam's dog, to visit. She was named 'treatment 18'. His consultant recognised the power of animal therapy, there was a chance Daisy could help Sam recover and we grabbed it. He also recognised that Daisy would give me and Sam's dad emotional support as well. Daisy was phenomenal. She trotted into the hospital like she was on a superhero mission, no-one was going to stop her getting to her big brother Sam. She wasn't phased going into PCCU despite all the strange sounds, sights and smells. With a room full of doctors and nurses, she hopped onto a chair and we managed to move Sam's hand for him so he could stroke her. She then settled onto his bed, with a big rug so she wouldn't damage the expensive mattress. Little did we know at the time this was the start of Daisy's Therapy Dog journey.
Reaching Out
We asked our Nottingham team to reach out to other neurology and PCCU consultants across the UK, and they unquestioningly did. Not that we were questioning their treatment of Sam, but in my mind the more brain power we had working on this, the better chance of success. They may have come across a treatment that we hadn’t heard of. From this we tried a number of innovative treatments including super high levels of phenobarbital, using isoflurane gas (used in theatre environment during operations) to achieve burst suppression, and cannabidiol.
Despair......Nothing was Working
The medical teams had reached a point, around six weeks into his treatment, where they needed to reduce Sam’s critical care drugs, as he could not remain on them indefinitely. The new strategy was that were not going to be able to stop his seizures and we needed to see if Sam could sustain his life and have any quality of life whilst having them. So, whilst his anaesthetic drugs were stopped, he would still continue receiving all his many anti-seizure drugs, and we were just going to treat the clinical seizures, i.e. the ones we could see.
So, Sam was taken off his Isoflurane gas, which had been sedating him and holding off the worst of his seizures. I was told by Sam's neurologist to be brave as it would most likely be heart breaking watching his seizures return. They were right it was the worst thing in the world watching my darling, sweet, gorgeous boy have his seizures return with a vengeance. His near constant seizing, drooling, and twitching. It was pure hell and torture to watch and it simply broke me. We had to document and time his seizures, but this was proving impossible as they were coming thick and fast, one after another. I asked my mum to buy lots of baby muslin's so I could put them around his face to try and catch as much drooling as I could so it wouldn’t hurt the skin on face; there was only so much suction he could take. I did my best to comfort him, to keep doing what I could to care for him. Reading his books to him, helping bath him, change his nappy, cover him in his body lotion that we loved to try and prevent bed sores and keep his circulation going, monitor him and in effect be an early alert for nurses to any changes in his condition or bodily functions. In my eyes I was Sam's one constant. I knew him better than anybody, I was with him from morning to night, and felt I knew what the 'norm' observations were for him, without even looking at his 24 hour observation sheet.
The Final Few Days
His cooling therapy blanket was removed, as we needed to see how he would cope without it. But his temperature started to become erratic again, clearly, he was not able to maintain his own body temperature.
His CFAM brain monitoring electrodes were removed, as we were only monitoring those clinical seizures we could see, they didn't want to see my eyes glued to the computer monitor showing his brain wave activities. He had a neurological exam by this neuro team, and the outcome of this was just catastrophic. He had no reactions in his legs or arms, and he didn’t have a gag reflex which you need to sustain breathing on your own. If you can’t gag you can choke. Sam's pupils were constantly dilated; not reacting to light. But in fairness they had been like this shortly after he was first admitted, around the time of his brain swelling.
He had his final MRI scan on the Wednesday 5 May, which had been delayed as he had an infection. The results were completely life shattering. His brain damage had evolved and was catastrophic. It was everywhere, in the middle of his brain, around the outside. It was likened to having super-fast dementia. When considering this alongside his neurological exam, all hope had been blasted away of Sam recovering, or having any quality of life. It felt like his brain had been eaten away. What ever it was wouldn't stop until there was nothing left of it.
Words are simply insufficient to explain how we felt. But all I could see was the suffering my darling brave baby boy was going through at just five years old, and it was just too much for a mother to bear.
A decision was made by the medical teams that Sam’s breathing tube, which was maintaining an airway for him, should be removed. Sam would make his own decision on whether he could survive or not. As parents we heartbreakingly supported this decision. As a mother, I did not want my baby boy to be left in a subconscious state, with no quality of life what so ever and we had all agreed there were simply no other treatments left to try.
Sam's Final Day
I stayed up with Sam through the night on the Friday evening, and it was heart wrenching. His seizures were just relentless despite all his anti-seizure meds, but it seemed Sam's body had gone haywire, he was now struggling to maintain a normal heartrate, blood pressure and his oxygen saturations kept plummeting. Our brilliant nurse and registrar were desperately trying to keep Sam as comfortable as possible, and I was still bathing him in his special body lotion to try and keep his skin soft and prevent bed sores. During the night his wonderful nurse worked utterly non-stop. Sam was starting to desaturate more often, he needed constant suctioning, one of his doctors was trying to do a heart trace on him, as his heart rhythm was now becoming erratic. I was helping her stick electrodes to his chest, but it was proving impossible, they were just slipping off (I think it was all the body lotion I put on him).
It feels surreal to write this, but I was not hysterically crying during the night, despite the fact that my child was highly likely going to die the following morning. I had gone passed that, my brain had now numbed me. It clearly knew it had to protect me, as otherwise I would not get through this. I had to do the right thing for my son, I had to be there for him. I had brought Sam into this world, and I would dam well make sure that I would be there right next to him, if he had to leave this world. Throughout the night I was simply trying to make Sam as comfortable as possible, trying to do the right thing for my son. All I could think of was that I did not want my son to be in a state worse than death e.g. in a minimally conscious state between life and death.
In the morning, Sam was given critical care meds to try and calm down some of his seizure activity and make him as comfortable as possible. We took handprints, in case the unthinkable happened and he wouldn’t be able to sustain his breathing when his breathing tube was removed.
Time that morning seemed to stand still whilst we prepared both Sam, and ourselves, to take out his breathing tube. It was removed around 1pm. For 90 minutes Sam tried to sustain his own life, but it just wasn’t possible. Whilst Sam's brain could trigger a breath, it could not control the muscles in his airway or maintain efficient breathing to sustain his life. His oxygen levels plummeted to 40%. Your brain does so much more than trigger a breath to breath, breathing is so much complex. So I sang Sam our special family song, repeatedly said his baby Jesus prayer that he knew so well, told him how loved he was, and told him how many people loved him over and over again. I told Sam that our strategy had now changed, mummy had kept her promise and sorted it all for him. Mummy and daddy were now giving him permission to leave us and go to baby Jesus, if that is what he needed to do. We told him not to be frightened, but to make his way into the light and he would be met by people who loved him so so so much.
And so our beautiful baby boy passed away in his mummy and daddy's arm on the 8 May 2021, exactly 5 years and 2 months old.
When Sam took his last breath, our world and life that we knew so well catastrophically shattered into a million pieces all around us. We then entered yet another new world of overwhelming grief, emptiness, numbness, desperation, and heart wrenching pain with the realisation that we would never again see our beautiful son, or hear his joyful voice his laugh and his giggles, or hear him call the words mummy and daddy, or feel his loving kisses and hugs, or see him write a card with I love you in, just because……well just because my precious boy felt like doing it.
To the world a little boy, to us the world. Briefly in our lives, forever in our hearts.
Sam's mummy
x
.png)
.png)




.png)

.png)

